Sciatica is one of the most common causes of back and leg pain, yet it remains a condition surrounded by confusion and misinformation. You may have heard people describe sciatica as a simple backache, but anyone who has experienced the condition knows that it can be much more than that. While many doctors offer sound advice and treatment options, there are some aspects of sciatica that are often overlooked or under-discussed. In this article, we’ll uncover the truth about sciatica, exploring the causes, symptoms, treatment options, and what your doctor may not tell you about managing this potentially debilitating condition.
What is Sciatica?
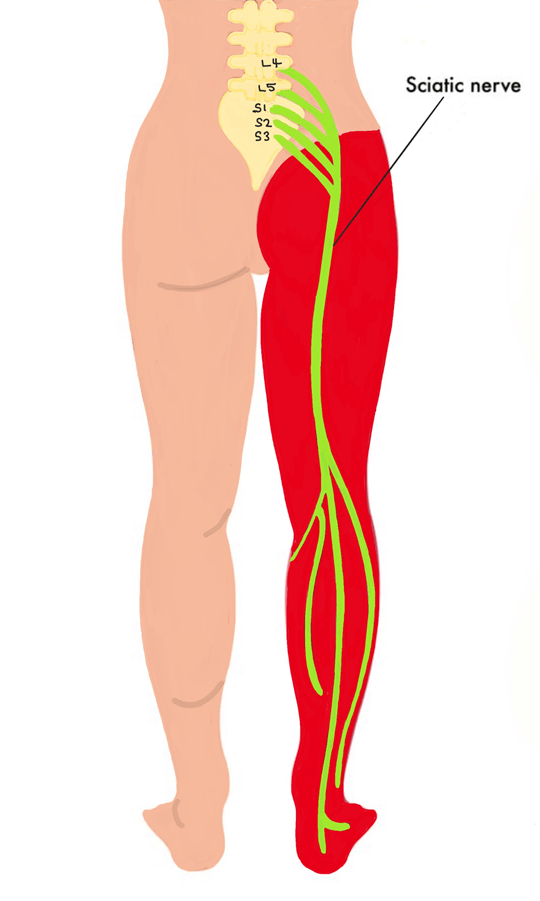
Before diving into what you may not hear from your doctor, it’s essential to understand what sciatica actually is. Sciatica refers to the pain that radiates along the path of the sciatic nerve, the largest nerve in the body. This nerve runs from your lower back, through your hips and buttocks, and down each leg. When the sciatic nerve is compressed or irritated, it can cause sharp, shooting pain, tingling, numbness, or even muscle weakness.
While sciatica is often referred to as a condition, it’s actually a symptom of an underlying issue such as a herniated disc, spinal stenosis, or piriformis syndrome. Understanding this distinction is important because treating sciatica involves addressing the root cause, not just the pain.
The Common Causes of Sciatica Your Doctor Will Mention
When you visit your doctor with complaints of sciatica, you’ll likely hear about the most common causes, which include:
- Herniated or slipped discs: When the cushioning discs between your vertebrae bulge or rupture, they can press on the sciatic nerve.
- Spinal stenosis: This is the narrowing of the spinal canal, often due to age-related changes, which can compress the sciatic nerve roots.
- Degenerative disc disease: As discs naturally degenerate over time, they lose their cushioning ability, leading to pressure on the sciatic nerve.
- Piriformis syndrome: The piriformis muscle, located deep in the buttocks, can spasm or tighten, irritating the sciatic nerve.
- Spondylolisthesis: This occurs when one vertebra slips forward over the one below it, potentially pinching the sciatic nerve.
These are legitimate causes, and they certainly explain many cases of sciatica. However, there’s more to the story.
What Your Doctor May Not Tell You About Sciatica
1. It’s Not Always a Structural Problem
One of the lesser-known facts about sciatica is that it’s not always due to a clear structural issue like a herniated disc. In some cases, sciatica can be triggered by muscle imbalances, postural problems, or even stress.
Tight muscles, particularly in the lower back and hips, can place pressure on the sciatic nerve, mimicking the symptoms of a disc problem. A sedentary lifestyle or poor posture, such as slouching at a desk, can also lead to nerve compression over time. In these cases, treating sciatica isn’t about invasive procedures or even painkillers – it’s about correcting muscular imbalances, improving posture, and maintaining an active lifestyle.
Moreover, stress can exacerbate pain and tension in the body, including in the lower back and hips. Chronic stress often leads to muscle tightness, which can indirectly contribute to sciatica symptoms.
2. Pain May Not Be Your Only Symptom
When most people think of sciatica, they think of pain shooting down the leg, but sciatica can present with a wide range of symptoms, some of which might not be immediately obvious. Along with the sharp, stabbing pain, you may experience:
- Numbness or tingling: Often described as a “pins and needles” sensation, this can occur in the buttocks, legs, or feet.
- Weakness: In some cases, sciatica can lead to muscle weakness in the leg, making it difficult to stand, walk, or move the affected limb.
- Loss of reflexes: A noticeable decrease in reflexes in the knee or ankle can occur when the sciatic nerve is compressed.
- Foot drop: In severe cases, you may experience difficulty lifting the front part of your foot when walking, a condition known as foot drop.
Because sciatica affects the largest nerve in the body, the symptoms can be more varied and widespread than just pain.

3. Pain Medications Aren’t Always the Best Solution
When you’re in pain, it’s natural to reach for medication. Most doctors will prescribe nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or even opioids to manage sciatica pain. However, while these medications can offer temporary relief, they do not address the underlying cause of the condition.
In fact, long-term reliance on pain medications can be harmful, as they only mask the pain and do little to resolve the root issue. For example, a muscle relaxant may ease the pain temporarily, but if your sciatica is due to muscle imbalances or poor posture, the relief will be short-lived.
What your doctor may not tell you is that lifestyle changes, physical therapy, and targeted exercises are often more effective long-term solutions for managing sciatica than medications. Strengthening the muscles that support the spine, stretching tight muscles, and improving posture can alleviate pressure on the sciatic nerve and provide lasting relief without the side effects associated with painkillers.
4. Surgery Isn’t Always Necessary
Sciatica can be incredibly painful, and in some cases, people feel desperate enough to consider surgery. While surgery is sometimes necessary for conditions like severe disc herniation or cauda equina syndrome (a rare, serious condition that requires immediate intervention), the truth is that most cases of sciatica can be resolved without surgery.
In fact, studies show that 90% of sciatica cases improve with non-surgical treatments such as physical therapy, lifestyle changes, and pain management techniques. Even when the cause of sciatica is a herniated disc, many people find relief through conservative treatment options like:
- Physical therapy: Targeted exercises to improve flexibility, strengthen muscles, and relieve pressure on the sciatic nerve.
- Chiropractic care: Spinal adjustments can help relieve nerve compression in some cases.
- Acupuncture: This traditional Chinese medicine technique has been shown to help reduce pain in some people with sciatica.
Surgery is typically considered a last resort, and it should only be pursued if conservative treatments fail or if the condition is causing severe, unmanageable symptoms such as loss of bladder or bowel control.
5. Your Lifestyle Plays a Huge Role in Recovery
What many people don’t realize is that sciatica can often be prevented or managed with lifestyle adjustments. If you’ve been diagnosed with sciatica or are at risk of developing it, you can make changes that significantly reduce your chances of experiencing flare-ups.
Here’s what your doctor might not emphasize:
- Stay active: While resting is important during acute flare-ups, prolonged inactivity can actually worsen sciatica. Low-impact activities like walking, swimming, and yoga can keep your muscles flexible and reduce pressure on the sciatic nerve.
- Core strengthening: A strong core helps support the spine and reduces the likelihood of nerve compression. Regular exercises to strengthen the abdominal and back muscles can prevent future episodes of sciatica.
- Maintain a healthy weight: Carrying excess weight, especially around the abdomen, can place added strain on the lower back, increasing the risk of sciatica.
- Ergonomics matter: Poor posture and improper ergonomics at work or home can contribute to sciatic nerve irritation. Adjusting your desk, chair, and computer screen to promote proper alignment can make a big difference in your long-term spinal health.
6. Emotional and Mental Health Impact Sciatica
It’s easy to focus solely on the physical aspects of sciatica, but emotional and mental health can play a significant role in both the severity of symptoms and the recovery process. Chronic pain conditions, like sciatica, can lead to feelings of frustration, anxiety, and even depression, which in turn can worsen the perception of pain.
Stress, in particular, can exacerbate physical symptoms. When we’re stressed, our muscles tense up, especially in the lower back, which can worsen sciatic nerve compression. Practicing stress management techniques like meditation, deep breathing exercises, or mindfulness can help alleviate both the emotional and physical toll of sciatica.
Engineer’s special movements fix back pain?
Have you had back pain or sciatica for years or decades?
This aeronautical engineer had both for 12 years until he took matters into his own hands.
==> Gentle “back and forth” movements fix back pain and sciatica
After stumbling on an inspiring 100-year-old German therapeutic “Movement Sequence”…
He used an engineering approach to create special new movements…
…and fixed 12 years of back pain in a matter of weeks.
These movements are gentle, so relaxing, and yet so shockingly effective at quickly fixing back pain.
(Even sciatica, spinal misalignment, disc herniation, pelvic tilt, tight back muscles, and more).
==> Engineer’s special movements fix back pain faster than anything else on the planet
