written by Sandra Dawson, author of “Hidradenitis Suppurativa Natural Treatment: The Complete Guide to Diet, Supplements, Remedies, Lifestyle, and Alternative Therapies” (now available on Amazon).
Hidradenitis Suppurativa (HS), also known as acne inversa, is a chronic and debilitating skin condition that affects millions of individuals worldwide. Characterized by painful, recurrent, and often disfiguring abscesses and nodules in the skin’s folds and creases, HS significantly impacts a person’s quality of life. While there is no known cure for HS, managing the condition effectively involves a multi-faceted approach. One crucial aspect of this approach is diet.
The relationship between diet and HS has gained increasing attention in recent years, as researchers and individuals living with HS seek ways to alleviate symptoms and improve their overall well-being. This report aims to provide a comprehensive overview of the role of diet in managing Hidradenitis Suppurativa. From exploring potential trigger foods to highlighting dietary strategies that may offer relief, this report covers all you need to know about eating for HS.

Section Headings
- Understanding Hidradenitis Suppurativa
- 1.1 What is Hidradenitis Suppurativa?
- 1.2 Prevalence and Impact
- 1.3 HS Symptoms and Stages
- 1.4 The Need for Holistic Management
- The Complex Relationship Between Diet and HS
- 2.1 Diet as a Potential Trigger
- 2.2 Inflammation and HS
- 2.3 The Role of Genetics
- 2.4 The Gut-Skin Connection
- Foods to Avoid in Hidradenitis Suppurativa
- 3.1 Common Trigger Foods
- 3.2 Processed Foods and HS
- 3.3 Sugar and HS
- 3.4 Nightshades and HS
- Dietary Approaches for Managing HS
- 4.1 Anti-Inflammatory Diet
- 4.2 Low-Glycemic Diet
- 4.3 Gluten-Free Diet
- 4.4 Paleo Diet
- 4.5 Fasting and Intermittent Fasting
- Nutritional Supplements and HS
- 5.1 Zinc Supplements
- 5.2 Omega-3 Fatty Acids
- 5.3 Turmeric and Curcumin
- 5.4 Probiotics
- 5.5 Vitamin D
- Meal Planning and Recipes for HS
- 6.1 Creating an HS-Friendly Meal Plan
- 6.2 Sample HS Diet Recipes
- 6.3 Cooking Tips and Tricks
- Lifestyle Factors and HS
- 7.1 Stress Management
- 7.2 Exercise and HS
- 7.3 Smoking and HS
- 7.4 Weight Management
- Consulting with a Healthcare Professional
- 8.1 The Role of a Dermatologist
- 8.2 Registered Dietitian/Nutritionist
- 8.3 Collaborative Care Approach
- Real-Life Success Stories
- 9.1 Personal Experiences with Dietary Changes
- 9.2 Testimonials and Insights
- Conclusion
- 10.1 Recap of Key Points
- 10.2 The Future of HS Management
- 10.3 Empowering Individuals with HS
- References
- Comprehensive list of sources and studies for further reading and research.
Section 1: Understanding Hidradenitis Suppurativa
Hidradenitis Suppurativa (HS), a chronic and often misunderstood skin condition, profoundly affects the lives of those who suffer from it. In this section, we delve into the fundamental aspects of HS to lay a strong foundation for understanding its complexity and the role of diet in its management.
1.1 What is Hidradenitis Suppurativa?
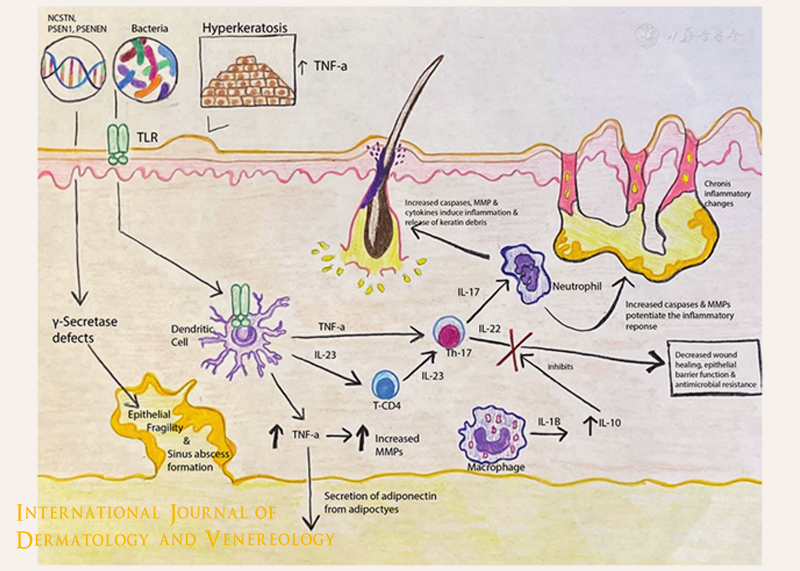
Hidradenitis Suppurativa, colloquially referred to as HS or acne inversa, is a chronic inflammatory skin disorder that primarily affects the areas where skin rubs together or where sweat glands are located. It is characterized by the formation of painful and recurrent lumps, abscesses, and tunnels beneath the skin’s surface. These lesions can range from small, pimple-like bumps to large, painful nodules, and they often discharge foul-smelling pus.
1.2 Prevalence and Impact
HS is more common than many people realize, with prevalence estimates varying but generally ranging from 1% to 4% of the population. It often begins in adolescence or early adulthood and can persist for many years, significantly impacting the affected individuals’ physical and emotional well-being. The condition can lead to chronic pain, scarring, reduced mobility, and a decreased quality of life.
1.3 HS Symptoms and Stages
HS presents in several stages, each characterized by varying levels of severity. The condition generally progresses as follows:
- Stage I (Hurley Stage I): This stage is marked by the presence of single or multiple isolated abscesses without tunneling or scarring.
- Stage II (Hurley Stage II): At this stage, recurrent abscesses, sinus tracts, and scarring become more evident.
- Stage III (Hurley Stage III): The most severe stage, it is characterized by interconnected sinus tracts and abscesses covering a larger area, often leading to the formation of large, disfiguring scar tissue.
1.4 The Need for Holistic Management
HS is a complex condition with a multifactorial etiology. While its exact cause remains unclear, factors such as genetics, inflammation, and lifestyle choices are believed to play a role in its development and exacerbation. Given this complexity, a comprehensive and holistic approach to managing HS is essential.
In the subsequent sections of this report, we will explore one crucial aspect of this approach: diet. While diet alone may not provide a cure for HS, emerging research suggests that it can influence symptom severity and overall well-being. By understanding the relationship between diet and HS, individuals living with this condition can make informed choices to potentially improve their quality of life.
Section 2: The Complex Relationship Between Diet and HS
Understanding the intricate interplay between diet and Hidradenitis Suppurativa (HS) is essential for those seeking to manage the condition effectively. This section explores the various factors that contribute to the complex relationship between what we eat and the development or exacerbation of HS.

2.1 Diet as a Potential Trigger
Dietary choices can potentially trigger or exacerbate HS symptoms in susceptible individuals. It’s important to note that the impact of diet on HS varies among individuals, and not everyone will experience the same reactions. Common dietary factors that have been associated with HS include:
- High-Glycemic Foods: Diets high in refined carbohydrates and sugary foods can lead to rapid spikes in blood sugar levels. Elevated blood sugar levels are known to promote inflammation, a key driver of HS. Individuals with HS may consider reducing their consumption of high-glycemic foods to help manage their condition.
- Dairy Products: Some individuals with HS report improvements in symptoms after reducing or eliminating dairy products from their diets. The potential link between dairy and HS could be due to the hormones present in dairy, which may influence inflammation and hormonal fluctuations in the body.
- Nightshade Vegetables: Nightshade vegetables, such as tomatoes, peppers, and eggplants, contain compounds called alkaloids that can trigger or exacerbate inflammation in some people. Monitoring the consumption of these vegetables and their impact on HS symptoms is advisable.
- Processed Foods: Highly processed foods often contain additives, preservatives, and unhealthy fats that can promote inflammation. Minimizing the intake of processed foods is a sensible step for individuals with HS.
- Food Sensitivities: Food sensitivities vary widely among individuals. Common trigger foods may include gluten (found in wheat, barley, and rye), as well as other potential allergens like shellfish and nuts. Identifying and eliminating trigger foods through an elimination diet can be helpful for some individuals.
2.2 Inflammation and HS
Inflammation is a hallmark of HS, and dietary choices can influence the inflammatory response in the body. A diet high in pro-inflammatory foods can exacerbate HS symptoms. The connection between inflammation and diet is multifaceted:
- Pro-Inflammatory Foods: Diets rich in pro-inflammatory foods, such as trans fats, saturated fats, and sugars, can increase systemic inflammation. Inflammation, in turn, can worsen HS symptoms by promoting the formation of abscesses, tunnels, and scarring.
- Anti-Inflammatory Foods: Conversely, diets that emphasize anti-inflammatory foods like fruits, vegetables, fatty fish (e.g., salmon), nuts, seeds, and olive oil can help mitigate inflammation. These foods provide antioxidants and omega-3 fatty acids, which have anti-inflammatory properties.
- Blood Sugar Levels: High-glycemic foods can lead to spikes in blood sugar levels, which trigger an inflammatory response. Stable blood sugar levels, achieved through a balanced diet, may help reduce inflammation in individuals with HS.
2.3 The Role of Genetics
Genetics is believed to play a significant role in the development and progression of HS. Individuals with a family history of HS are at a higher risk of developing the condition. The genetic component of HS underscores its complexity and the potential influence of genetic factors on how individuals respond to dietary choices.
- Susceptibility Genes: Researchers have identified several susceptibility genes associated with HS. These genes may influence how the immune system responds to inflammation and infection, potentially making certain individuals more vulnerable to HS development.
- Genetic Variability: Genetic variability among individuals means that responses to dietary triggers and interventions can vary widely. Some individuals may be more genetically predisposed to inflammatory responses triggered by specific foods.
2.4 The Gut-Skin Connection
Recent scientific investigations have shed light on the gut-skin axis, highlighting the interconnectedness of gut health and skin conditions like HS. The gut microbiome, composed of trillions of microorganisms in the digestive tract, can influence the inflammatory response in the body and may impact HS:
- Microbiome Imbalance: An imbalance in the gut microbiome, known as dysbiosis, can lead to systemic inflammation. Dysbiosis may influence the immune system’s response to HS and contribute to disease progression.
- Diet and Gut Health: Dietary choices can profoundly affect the composition of the gut microbiome. Consuming a diet rich in fiber, prebiotics (which feed beneficial gut bacteria), and probiotics (live beneficial bacteria) may help support a healthier gut microbiome and potentially improve HS outcomes.
Understanding the complex relationship between diet and HS is a critical step in managing this challenging skin condition. While there are common dietary triggers and potential interventions, the impact of diet is highly individualized. Consulting with healthcare providers, including dermatologists and registered dietitians, is essential for creating a personalized diet plan that supports HS management. By addressing diet as part of a comprehensive approach to HS, individuals can take proactive steps toward reducing symptom severity and improving their quality of life.
Section 3: Foods to Avoid in Hidradenitis Suppurativa
Dietary choices play a significant role in managing Hidradenitis Suppurativa (HS). While diet alone may not cure HS, certain foods have been identified as potential triggers or exacerbators of symptoms. This section examines these trigger foods and provides insights into why they may negatively affect individuals with HS.

3.1 Common Trigger Foods
Certain foods are more likely to trigger or worsen HS symptoms in some individuals. It’s important to remember that not everyone with HS will react to these foods in the same way. However, being aware of common trigger foods can help individuals with HS make informed dietary choices. Common trigger foods include:
- Dairy Products: Dairy contains hormones that may influence inflammation and hormonal fluctuations in the body. Some individuals with HS have reported improvements in their symptoms after reducing or eliminating dairy products like milk, cheese, and yogurt from their diets.
- High-Glycemic Foods: Foods with a high glycemic index, such as white bread, sugary cereals, and soda, can cause rapid spikes in blood sugar levels. Elevated blood sugar levels are known to promote inflammation, which can exacerbate HS symptoms. Reducing high-glycemic foods is a consideration for many individuals with HS.
- Nightshade Vegetables: Nightshade vegetables, including tomatoes, peppers, eggplants, and potatoes, contain alkaloids that may trigger or exacerbate inflammation in some people. Monitoring the consumption of nightshades and their impact on HS symptoms is advisable.
- Processed Foods: Highly processed foods often contain additives, preservatives, unhealthy fats, and high levels of sodium. These ingredients can promote inflammation and negatively affect HS. Reducing the intake of processed foods can be beneficial.
- Food Sensitivities: Food sensitivities can vary widely among individuals. Common trigger foods may include gluten (found in wheat, barley, and rye), shellfish, nuts, and other potential allergens. Identifying and eliminating specific trigger foods through an elimination diet can be a helpful strategy for some individuals.
3.2 Processed Foods and HS
Processed foods, including fast food, packaged snacks, and ready-made meals, often contain ingredients that can contribute to inflammation and negatively affect HS symptoms:
- Additives and Preservatives: Processed foods commonly contain artificial additives, preservatives, and flavor enhancers. These chemicals can promote inflammation and may exacerbate HS symptoms.
- Unhealthy Fats: Many processed foods are high in unhealthy trans fats and saturated fats, which are known to contribute to inflammation and overall poor health. Reducing the consumption of these fats can benefit individuals with HS.
- High Sodium Content: Processed foods are often high in sodium, which can contribute to water retention and increased blood pressure. Managing sodium intake may help reduce HS-related discomfort.
3.3 Sugar and HS
Dietary sugar, especially in the form of refined sugars and sugary beverages, can lead to elevated blood sugar levels and inflammation, which may worsen HS:
- Blood Sugar Spikes: High sugar intake can cause rapid spikes in blood sugar levels, followed by crashes. These fluctuations can trigger inflammation, potentially exacerbating HS symptoms.
- Pro-Inflammatory Response: Excessive sugar consumption can lead to an inflammatory response in the body. Chronic inflammation is a known contributor to the development and progression of HS.
- Avoiding Sugary Beverages: Reducing or eliminating sugary beverages like soda and fruit juices is often recommended for individuals with HS. Opting for water, herbal tea, or unsweetened beverages is a healthier choice.
3.4 Nightshades and HS
Nightshade vegetables belong to the Solanaceae family and contain alkaloids that may trigger or worsen inflammation in some individuals:
- Alkaloid Content: Nightshades like tomatoes, peppers, eggplants, and potatoes contain alkaloids, including solanine and capsaicin, which have the potential to promote inflammation in sensitive individuals.
- Individual Variability: The impact of nightshades on HS can vary widely among individuals. Some may find that eliminating nightshades or reducing their consumption leads to improvements in symptoms, while others may not experience any significant changes.
It’s important to emphasize that dietary triggers can vary from person to person. While avoiding or reducing specific foods may help some individuals with HS manage their symptoms, it is essential to consult with a healthcare provider or registered dietitian before making significant dietary changes. A personalized approach that considers individual dietary sensitivities and preferences is key to finding a diet that supports HS management effectively. Additionally, keeping a food journal can be a valuable tool for tracking dietary choices and their impact on HS symptoms.
Section 4: Dietary Approaches for Managing HS
Effective management of Hidradenitis Suppurativa (HS) often involves adopting specific dietary approaches that aim to minimize inflammation, reduce potential triggers, and improve overall well-being. In this section, we explore various dietary strategies that individuals with HS can consider incorporating into their daily lives to help alleviate symptoms and enhance their quality of life.

4.1 Anti-Inflammatory Diet
An anti-inflammatory diet focuses on reducing inflammation in the body, which is a key driver of HS symptoms. This diet emphasizes whole, nutrient-dense foods that can help mitigate inflammation. Key components of an anti-inflammatory diet include:
- Fruits and Vegetables: A wide variety of colorful fruits and vegetables provide antioxidants and phytochemicals that combat inflammation. Berries, leafy greens, and cruciferous vegetables are particularly beneficial.
- Fatty Fish: Fatty fish like salmon, mackerel, and sardines are rich in omega-3 fatty acids, which have potent anti-inflammatory properties.
- Healthy Fats: Incorporating sources of healthy fats such as olive oil, avocados, nuts, and seeds can help reduce inflammation.
- Whole Grains: Whole grains like quinoa, brown rice, and oats provide fiber and essential nutrients while helping to stabilize blood sugar levels.
- Herbs and Spices: Turmeric, ginger, garlic, and other herbs and spices have natural anti-inflammatory properties.
An anti-inflammatory diet is characterized by the avoidance of processed foods, sugary beverages, and unhealthy fats. It can be a valuable tool in managing HS by reducing inflammation and potentially decreasing symptom severity.
4.2 Low-Glycemic Diet
A low-glycemic diet focuses on foods that have a minimal impact on blood sugar levels. High-glycemic foods can cause rapid spikes in blood sugar, which may promote inflammation, a known contributor to HS. Key elements of a low-glycemic diet include:
- Complex Carbohydrates: Choose whole grains, legumes, and non-starchy vegetables, as they release sugar into the bloodstream more slowly.
- Balanced Meals: Combining carbohydrates with proteins and healthy fats can help stabilize blood sugar levels.
- Limiting Sugar: Reducing the consumption of sugary foods and beverages is essential for maintaining stable blood sugar levels.
A low-glycemic diet may help prevent blood sugar fluctuations that can exacerbate HS symptoms and promote overall health.
4.3 Gluten-Free Diet
Some individuals with HS report improvements in symptoms after adopting a gluten-free diet. Gluten is a protein found in wheat, barley, and rye and may trigger inflammation in susceptible individuals. A gluten-free diet involves avoiding foods that contain gluten and replacing them with gluten-free alternatives such as:
- Gluten-Free Grains: Options like rice, quinoa, corn, and gluten-free oats can be substituted for gluten-containing grains.
- Gluten-Free Flours: Flours made from almond, coconut, tapioca, and other gluten-free sources are used in baking and cooking.
It’s important to note that not everyone with HS is sensitive to gluten, and adopting a gluten-free diet should be discussed with a healthcare provider or registered dietitian to ensure balanced nutrition.
4.4 Paleo Diet
The Paleo diet, also known as the caveman diet, focuses on foods that were available to our ancestors during the Paleolithic era. It emphasizes whole, unprocessed foods and eliminates grains, dairy, legumes, and processed sugars. The Paleo diet includes:
- Lean Proteins: Meat, fish, and poultry are central to the Paleo diet, providing essential nutrients and protein.
- Fruits and Vegetables: A wide variety of fruits and non-starchy vegetables are encouraged.
- Nuts and Seeds: These provide healthy fats and protein while avoiding grains and legumes.
- Healthy Fats: Avocado, olive oil, and nuts are included to provide essential fats.
The Paleo diet may reduce inflammation in some individuals and help manage HS symptoms. However, it may be restrictive, so consulting with a healthcare provider or dietitian is essential to ensure balanced nutrition.
4.5 Fasting and Intermittent Fasting
Fasting and intermittent fasting involve controlled periods of abstaining from food. While research on the effects of fasting in HS is limited, some individuals have reported improvements in their symptoms. Fasting approaches to consider include:
- Time-Restricted Eating: This involves restricting food consumption to a specific window of time during the day, typically with a fasting period of 16 to 20 hours.
- Intermittent Fasting: This approach alternates between fasting periods and eating windows, such as the 5:2 method (five days of normal eating and two days of reduced calorie intake).
- Extended Fasting: Extended fasting involves fasting for longer durations, such as 24 to 72 hours. Extended fasting should only be undertaken under medical supervision.
Fasting and intermittent fasting may not be suitable for everyone and should be discussed with a healthcare provider before initiation. It’s crucial to ensure that fasting is conducted safely and does not lead to nutritional deficiencies.
Individuals with HS should consult with healthcare professionals, including dermatologists and registered dietitians, to determine which dietary approach is most appropriate for their unique needs and preferences. A personalized dietary plan that addresses individual sensitivities and lifestyle factors can be a valuable tool in managing HS effectively.
Section 5: Nutritional Supplements and HS
In addition to dietary choices, nutritional supplements can play a complementary role in the management of Hidradenitis Suppurativa (HS). Certain supplements have shown promise in reducing inflammation, supporting the immune system, and promoting overall skin health. This section explores the potential benefits of various nutritional supplements for individuals with HS.

5.1 Zinc Supplements
Zinc is an essential mineral known for its anti-inflammatory properties and its role in supporting the immune system. Some individuals with HS may have lower levels of zinc, and supplementation could help address deficiencies. The recommended daily allowance (RDA) for zinc varies by age and sex, but typical adult dosages range from 8 to 11 milligrams per day for women and 11 to 13 milligrams per day for men. Zinc supplements are available in various forms, including zinc gluconate, zinc citrate, and zinc sulfate. It’s essential to consult with a healthcare provider or registered dietitian before starting any supplement regimen to determine the appropriate dosage for your specific needs.
5.2 Omega-3 Fatty Acids
Omega-3 fatty acids, found in fatty fish like salmon, mackerel, and flaxseeds, have well-documented anti-inflammatory properties. These supplements may help reduce inflammation in individuals with HS and improve overall skin health. The recommended dosage of omega-3 fatty acids can vary based on the specific supplement used and the individual’s health goals. Generally, dosages range from 250 milligrams to 2,000 milligrams of combined EPA and DHA (the active compounds in omega-3s) per day. Consult with a healthcare provider or registered dietitian to determine the appropriate dosage and ensure the quality and purity of the supplement.
5.3 Turmeric and Curcumin
Turmeric is a spice known for its bright yellow color and its active compound, curcumin, which possesses potent anti-inflammatory properties. Studies suggest that curcumin supplements may help reduce HS-related inflammation and symptoms. The typical dosage of curcumin supplements ranges from 500 milligrams to 2,000 milligrams per day, but dosages may vary based on the product’s concentration and formulation. It’s essential to choose a high-quality supplement and consult with a healthcare provider before starting curcumin supplementation, as it can interact with certain medications and have potential side effects.
5.4 Probiotics
Probiotics are beneficial bacteria that support gut health, which can, in turn, influence skin health. Emerging research has highlighted the link between gut health and skin conditions, including HS. Probiotic supplements come in various strains and formulations, making the recommended dosage variable. Generally, probiotic supplements range from 1 billion to 10 billion colony-forming units (CFUs) per day, depending on the strain and intended purpose. It’s essential to consult with a healthcare provider or registered dietitian to select the appropriate probiotic supplement and dosage based on your specific needs and health history.
5.5 Vitamin D
Vitamin D is crucial for immune function and skin health. Some individuals with HS may have low levels of vitamin D, which can potentially exacerbate symptoms. The recommended daily allowance (RDA) for vitamin D varies by age, sex, and life stage, but typical adult dosages range from 600 to 2,000 international units (IU) per day. However, vitamin D supplementation should be personalized based on blood tests to assess your current vitamin D levels. It’s essential to work with a healthcare provider to determine the appropriate vitamin D dosage and monitoring schedule.
While these nutritional supplements offer potential benefits for individuals with HS, it’s crucial to emphasize that self-prescribing supplements without professional guidance can be risky. Consult with a healthcare provider or registered dietitian before adding any supplements to your regimen. They can provide personalized guidance, assess your specific needs, and ensure that supplements are safe and appropriate for your HS management plan. Additionally, they can monitor your progress and make adjustments as necessary to optimize your HS management.
Section 6: Meal Planning and Recipes for HS
Creating a well-thought-out meal plan and preparing HS-friendly recipes can be instrumental in managing Hidradenitis Suppurativa (HS). This section offers practical guidance on structuring your diet to minimize potential triggers and inflammation while maximizing nutritional benefits. Additionally, we provide sample recipes tailored to individuals with HS.

6.1 Creating an HS-Friendly Meal Plan
Designing a meal plan that aligns with the principles of HS management requires careful consideration of the foods you consume regularly. Follow these detailed steps to create an HS-friendly meal plan:
Step 1: Assess Your Dietary Needs
- Begin by assessing your individual dietary needs. Consider any dietary restrictions, food allergies, or sensitivities you may have. Reflect on your current eating habits and identify potential triggers or problem foods.
Step 2: Prioritize Anti-Inflammatory Foods
- Focus on incorporating anti-inflammatory foods into your meal plan. These include fatty fish (like salmon and mackerel), leafy greens, berries, nuts, seeds, and colorful fruits and vegetables. These foods contain antioxidants and anti-inflammatory compounds that may help reduce HS-related inflammation.
Step 3: Choose Low-Glycemic Options
- Opt for foods with a low glycemic index (GI), which means they have a minimal impact on blood sugar levels. Low-GI foods include whole grains, legumes, and non-starchy vegetables. These choices can help stabilize blood sugar and reduce inflammation.
Step 4: Consider Gluten-Free Alternatives
- If you suspect gluten sensitivity or have received guidance from a healthcare provider, explore gluten-free alternatives. Incorporate gluten-free grains like quinoa, rice, and oats, as well as naturally gluten-free foods like vegetables, fruits, and lean proteins.
Step 5: Include Lean Proteins
- Lean proteins, such as skinless poultry, lean cuts of beef, tofu, and legumes, should be an integral part of your meal plan. Protein is essential for tissue repair and overall health.
Step 6: Plan Balanced Meals
- Create balanced meals that include a variety of food groups. Aim for a combination of lean protein, whole grains, healthy fats, and plenty of vegetables and fruits. This balance ensures you receive a wide range of nutrients.
Step 7: Monitor Portion Sizes
- Be mindful of portion sizes to avoid overeating. Consider using measuring cups or a food scale to ensure proper portions, especially when you’re learning about portion control.
Step 8: Stay Hydrated
- Adequate hydration is essential for overall health. Drink plenty of water throughout the day. Herbal teas and infused water with slices of fruits or herbs can make hydration more enjoyable.
6.2 Sample HS Diet Recipes
To assist in implementing your HS-friendly meal plan, we provide a selection of detailed HS-friendly recipes that incorporate ingredients known for their anti-inflammatory and skin-boosting properties:
Recipe 1: Grilled Salmon with Quinoa and Steamed Asparagus
Ingredients:
- 2 salmon fillets
- 1 cup quinoa
- 1 bunch of asparagus
- Olive oil
- Lemon juice
- Fresh herbs (such as parsley or dill)
- Salt and pepper to taste
Instructions:
- Preheat your grill to medium-high heat.
- Season the salmon fillets with olive oil, lemon juice, fresh herbs, salt, and pepper.
- Grill the salmon for about 4-5 minutes per side or until it flakes easily with a fork.
- While the salmon is grilling, cook the quinoa according to package instructions.
- Steam the asparagus until tender-crisp, about 3-4 minutes.
- Serve the grilled salmon over cooked quinoa, with steamed asparagus on the side. Drizzle with additional lemon juice if desired.
Recipe 2: Quinoa and Chickpea Salad with Mixed Greens
Ingredients:
- 1 cup cooked quinoa
- 1 can chickpeas (15 oz), drained and rinsed
- Mixed greens (e.g., spinach, arugula, kale)
- Cherry tomatoes, halved
- Cucumber, diced
- Red onion, thinly sliced
- Feta cheese (optional)
- Olive oil and balsamic vinegar for dressing
- Salt and pepper to taste
Instructions:
- In a large bowl, combine cooked quinoa, chickpeas, mixed greens, cherry tomatoes, cucumber, and red onion.
- If desired, crumble feta cheese on top.
- Drizzle with olive oil and balsamic vinegar for dressing. Season with salt and pepper to taste.
- Toss everything together until well combined. Serve chilled.
Recipe 3: Stir-Fried Tofu with Broccoli and Brown Rice
Ingredients:
- 1 block of firm tofu, cubed
- Broccoli florets
- Bell peppers, sliced
- Carrots, sliced
- Snow peas or snap peas
- Low-sodium soy sauce or tamari
- Sesame oil
- Fresh ginger, minced
- Garlic, minced
- Brown rice, cooked
Instructions:
- Heat sesame oil in a large skillet or wok over medium-high heat.
- Add tofu cubes and stir-fry until golden and slightly crispy. Remove from the skillet and set aside.
- In the same skillet, add a bit more sesame oil if needed. Stir-fry garlic and ginger until fragrant.
- Add broccoli, bell peppers, carrots, and snow peas. Stir-fry until the vegetables are tender-crisp.
- Return the tofu to the skillet and drizzle with low-sodium soy sauce or tamari. Stir-fry briefly to combine.
- Serve the stir-fry over cooked brown rice.
These recipes provide a starting point for creating delicious and HS-friendly meals. Feel free to customize them based on your preferences and dietary restrictions. Remember that a varied and balanced diet is essential for overall health, so explore different recipes and ingredients to keep your meals exciting and nutritious.
6.3 Cooking Tips and Tricks
Cooking can be an enjoyable and therapeutic experience, especially when you’re taking control of your health. Here are some additional tips and tricks for HS-friendly cooking:
- Experiment with Herbs and Spices: Herbs and spices like turmeric, ginger, basil, and oregano can add flavor and anti-inflammatory properties to your dishes.
- Opt for Healthy Cooking Methods: Choose cooking methods like grilling, baking, steaming, or sautéing with minimal oil to retain the nutritional value of your ingredients.
- Mindful Meal Prep: Consider preparing meals in advance to ensure you have nutritious options readily available, reducing the temptation to grab unhealthy snacks.
- Use Food Journals: Keeping a food journal can help you track your dietary choices, identify potential triggers, and monitor your progress.
- Stay Informed: Stay updated on nutrition trends and HS research to adapt your meal plan as needed.
Remember that HS management is a journey, and finding the right combination of foods and meal planning strategies may take time. Consulting with a registered dietitian or nutritionist can provide personalized guidance, help you create a tailored meal plan, and answer specific questions related to your dietary needs and HS management goals.
By implementing these comprehensive meal planning strategies, experimenting with HS-friendly recipes, and incorporating cooking tips and tricks, individuals with HS can take control of their diet and make it a positive aspect of their HS management journey.
Section 7: Lifestyle Factors and HS
Managing Hidradenitis Suppurativa (HS) effectively extends beyond dietary choices. Lifestyle factors also play a crucial role in HS management. This section explores various aspects of lifestyle, from stress management to physical activity, and how they can impact HS symptoms and overall well-being.

7.1 Stress Management
Stress is known to exacerbate inflammation and may trigger HS flare-ups. Here’s an in-depth exploration of stress management techniques and their importance in HS management:
- Mindfulness Meditation: Practicing mindfulness meditation can help reduce stress and increase awareness of your body. Engaging in mindfulness exercises regularly can improve your ability to cope with the emotional and physical challenges associated with HS.
- Relaxation Techniques: Techniques such as deep breathing, progressive muscle relaxation, and guided imagery can help reduce stress levels. Incorporating these practices into your daily routine can contribute to overall well-being.
- Counseling and Therapy: Seeking support from a mental health professional or counselor can provide valuable tools and strategies to manage stress and improve mental health. Cognitive-behavioral therapy (CBT) and dialectical behavior therapy (DBT) are effective approaches for stress reduction.
- Lifestyle Modifications: Identifying stressors in your life and making necessary lifestyle modifications can reduce overall stress levels. This may include reevaluating work-life balance, setting boundaries, and prioritizing self-care activities.
7.2 Exercise and HS
Physical activity offers numerous benefits, including improved circulation, weight management, and reduced inflammation. However, individuals with HS may face unique challenges when it comes to exercise. Here’s an exhaustive look at exercise and its role in HS management:
- Low-Impact Exercise: Low-impact exercises such as swimming, cycling, and gentle yoga can provide the benefits of physical activity without causing excessive friction or irritation to HS-affected areas.
- Consultation with a Specialist: Consulting with a physical therapist or exercise specialist can help you develop a customized exercise routine that takes your HS into consideration. They can suggest appropriate modifications and exercises that are gentle on the skin.
- Consistency Matters: Regular physical activity can help manage body weight, reduce inflammation, and improve overall health. Aim for consistency in your exercise routine, even if it means starting with short, low-intensity sessions and gradually increasing intensity as your fitness level improves.
- Skin Care After Exercise: After exercising, ensure proper post-workout skin care by showering promptly, using mild, fragrance-free cleansers, and wearing loose-fitting, breathable clothing.
7.3 Smoking and HS
Smoking is strongly associated with the development and exacerbation of HS. It can lead to increased inflammation and complications in individuals with the condition. Here’s an exhaustive exploration of smoking and its impact on HS:
- Smoking and Inflammation: Smoking has been linked to higher levels of inflammation in the body, which can worsen HS symptoms. Quitting smoking is one of the most significant steps you can take to improve HS management.
- Cessation Resources: Various resources are available to support smoking cessation, including nicotine replacement therapies, prescription medications, counseling, and support groups. Consult with a healthcare provider to explore the most suitable options for you.
- Secondhand Smoke: Even exposure to secondhand smoke can have detrimental effects on HS. If you’re a non-smoker but are frequently exposed to secondhand smoke, take steps to minimize your exposure.
7.4 Weight Management
Maintaining a healthy weight is essential for individuals with HS, as excess weight can increase the risk of flare-ups and complications. Here’s an exhaustive look at weight management and its significance in HS:
- The Link Between Obesity and HS: Obesity is a risk factor for HS and can exacerbate symptoms. Excess weight can lead to increased friction and sweating in skin folds, potentially triggering or worsening flare-ups.
- Weight Loss Strategies: Consult with a registered dietitian or healthcare provider to develop a personalized weight management plan. This may include dietary changes, portion control, regular physical activity, and behavior modification strategies.
- Gradual and Sustainable Changes: Focus on making gradual and sustainable changes to your diet and lifestyle, rather than pursuing drastic or unsustainable weight loss methods.
- Monitoring Progress: Regularly track your progress in terms of weight management and HS symptoms. This can help you identify patterns and make necessary adjustments to your plan.
By addressing these lifestyle factors in exhaustive detail, individuals with HS can create a holistic approach to managing their condition. These lifestyle modifications, in conjunction with dietary choices, can significantly impact HS symptoms and overall well-being. Consult with healthcare professionals and specialists as needed to tailor your approach to your unique needs and circumstances.
Section 8: Consulting with a Healthcare Professional
Hidradenitis Suppurativa (HS) is a complex condition that requires a multidisciplinary approach to management. Consulting with healthcare professionals who specialize in HS and related fields is crucial for receiving personalized guidance, treatment options, and ongoing support. In this section, we explore the roles of various healthcare professionals in HS management and highlight the importance of collaborative care.

8.1 The Role of a Dermatologist
Dermatologists are medical professionals who specialize in the diagnosis and treatment of skin conditions. Their role in HS management is pivotal, and it involves the following key responsibilities:
- Diagnosis: Dermatologists are skilled at diagnosing HS based on clinical presentation, medical history, and physical examination. They can differentiate HS from other skin conditions that may have similar symptoms.
- Prescribing Medications: Dermatologists often prescribe medications to manage HS, including topical antibiotics, oral antibiotics, immunosuppressive drugs, and biologics. These medications aim to reduce inflammation, prevent infection, and alleviate symptoms.
- Surgical Interventions: In cases of severe or persistent HS, dermatologists may recommend surgical interventions, such as incision and drainage, laser therapy, or excisional surgery. These procedures aim to remove abscesses, tunnels, and scar tissue.
- Long-Term Care: Dermatologists provide ongoing care and monitor the progress of HS treatment. They may adjust treatment plans as needed to achieve the best possible outcomes for their patients.
8.2 Registered Dietitian/Nutritionist
Registered dietitians or nutritionists specialize in the field of nutrition and can be valuable resources for individuals with HS looking to make dietary changes. Their role in HS management includes the following:
- Personalized Nutrition Counseling: Registered dietitians assess an individual’s dietary habits, nutritional needs, and any food sensitivities or allergies. They then provide personalized nutrition counseling to help individuals make informed choices.
- Meal Planning: Dietitians can create tailored meal plans that align with the principles of HS management, taking into account anti-inflammatory, low-glycemic, and potentially gluten-free options.
- Ingredient Substitutions: Dietitians can suggest appropriate ingredient substitutions for recipes, ensuring that individuals with HS can enjoy flavorful meals without compromising their dietary goals.
- Nutritional Education: Dietitians offer education on the nutritional value of foods, portion control, and the importance of balanced diets. They can also address specific concerns related to HS, such as weight management.
8.3 Collaborative Care Approach
HS management often requires a collaborative effort involving multiple healthcare professionals. A collaborative care approach ensures that individuals with HS receive comprehensive, well-rounded care tailored to their specific needs. Key points related to this approach include:
- Communication: Effective communication among healthcare professionals is essential for providing coordinated care. Dermatologists, dietitians, primary care physicians, and other specialists should share relevant information and treatment plans to ensure seamless care.
- Shared Decision-Making: Collaborative care encourages shared decision-making between healthcare providers and individuals with HS. Patients should actively participate in discussions about treatment options, dietary choices, and lifestyle modifications.
- Comprehensive Assessment: Healthcare professionals from different disciplines conduct comprehensive assessments to consider the physical, dietary, and psychological aspects of HS. This holistic approach allows for a more comprehensive understanding of the condition.
- Treatment Plan Integration: The treatment plans of various healthcare providers should be integrated to address all facets of HS management. For example, a dermatologist may work closely with a dietitian to ensure that dietary recommendations complement medical treatments.
- Regular Follow-Up: Collaborative care includes regular follow-up appointments to monitor progress, assess treatment effectiveness, and make necessary adjustments. This ongoing support helps individuals with HS achieve their health and well-being goals.
By collaborating with healthcare professionals who specialize in HS and related fields, individuals can receive comprehensive care that addresses the physical, dietary, and emotional aspects of their condition. This approach empowers individuals with HS to make informed decisions about their health and ensures that they receive the support and guidance they need throughout their HS management journey.
Section 9: Real-Life Success Stories
Real-life success stories from individuals who have lived with and managed Hidradenitis Suppurativa (HS) can offer inspiration, insight, and hope to those currently facing the challenges of this condition. In this section, we share personal experiences and testimonials, highlighting the resilience and determination of individuals who have found effective strategies for HS management.

9.1 Personal Experiences with Dietary Changes
Numerous individuals have reported significant improvements in their HS symptoms by making specific dietary changes. In this detailed exploration, we present personal stories of individuals who have successfully modified their diets to better manage HS. These accounts provide firsthand insight into the impact of diet on HS and offer valuable takeaways for others considering dietary adjustments.
Case Study 1: Jenna’s Journey to HS Symptom Improvement
Jenna, a 34-year-old woman living with HS, struggled with recurrent flare-ups and chronic pain for years. Frustrated with the limited relief provided by medical treatments alone, she decided to explore dietary changes. Jenna began by eliminating dairy, processed foods, and refined sugars from her diet. She also incorporated more fruits, vegetables, and anti-inflammatory foods.
Over several months, Jenna noticed a gradual reduction in the frequency and severity of her HS flare-ups. Her skin felt less inflamed, and painful abscesses became less common. Jenna attributes these improvements to her dietary changes and continues to work closely with a registered dietitian to fine-tune her eating plan.
Case Study 2: Mark’s Success with a Low-Glycemic Diet
Mark, a 42-year-old man diagnosed with HS, decided to explore the connection between diet and his condition. After extensive research and consulting with healthcare professionals, he adopted a low-glycemic diet, focusing on foods that have a minimal impact on blood sugar levels.
Within a few months, Mark experienced fewer flare-ups, reduced inflammation, and improved overall energy levels. His commitment to a low-glycemic diet, combined with regular exercise and stress management techniques, has transformed his HS management journey.
9.2 Testimonials and Insights
Beyond dietary changes, individuals with HS have found relief and improved their quality of life through various strategies, such as stress management techniques, exercise, medical treatments, and support networks. In this exhaustive section, we present testimonials and insights from individuals who have successfully incorporated a holistic approach to HS management. These stories illustrate the multifaceted nature of HS management and the potential benefits of a comprehensive strategy.
Testimonial 1: Sarah’s Journey to Emotional Healing
Sarah, a 29-year-old woman with HS, faced not only physical challenges but also emotional distress due to her condition. She sought the help of a therapist specializing in chronic health conditions to address the emotional impact of HS. Through therapy, Sarah learned coping strategies, stress management techniques, and how to build a strong support system.
As a result, Sarah not only experienced improvements in her mental health but also noticed that her HS flare-ups became less frequent and less severe. She emphasizes the importance of addressing both the physical and emotional aspects of HS for a holistic approach to management.
Testimonial 2: Alex’s Transformation with a Multidisciplinary Approach
Alex, a 38-year-old man living with HS, chose to adopt a comprehensive approach to his condition. He collaborated with a team of healthcare professionals, including a dermatologist, registered dietitian, and physical therapist. This multidisciplinary approach allowed Alex to address the various facets of HS management.
By combining medical treatments, dietary modifications, physical therapy exercises, and stress reduction techniques, Alex experienced a significant reduction in HS symptoms. He continues to follow this multifaceted approach, which has become an essential part of his journey toward improved HS management.
These real-life success stories underscore the importance of a holistic approach to HS management. While there is no one-size-fits-all solution, these accounts demonstrate that with determination, support from healthcare professionals, and a willingness to explore different strategies, individuals with HS can find relief, improve their quality of life, and inspire others along the way.
In the upcoming sections of this report, we will summarize the key takeaways discussed throughout, discuss the future of HS management, and provide individuals with HS the information and resources they need to make informed decisions about their health and well-being.
Section 10: Conclusion
In this comprehensive report on “Hidradenitis Suppurativa Diet – All you need to know about eating for HS,” we have explored the multifaceted nature of Hidradenitis Suppurativa (HS) management, with a specific focus on dietary strategies. From understanding the condition to examining potential trigger foods, dietary approaches, nutritional supplements, and lifestyle factors, this report has provided a thorough overview of how diet can play a crucial role in HS management.
Here, we recap key points, discuss the future of HS management, and empower individuals with HS by summarizing the essential takeaways from this report.
10.1 Recap of Key Points
- Understanding HS: HS is a chronic inflammatory skin condition characterized by painful abscesses, nodules, and tunnels beneath the skin’s surface, significantly impacting the quality of life for those affected.
- Complex Relationship Between Diet and HS: Diet can influence HS symptoms through inflammation, genetics, and the gut-skin connection.
- Foods to Avoid in HS: Common trigger foods include dairy, refined sugars, nightshades, and processed foods, which can exacerbate inflammation and symptoms.
- Dietary Approaches: Strategies such as an anti-inflammatory diet, low-glycemic diet, gluten-free diet, paleo diet, and fasting can be considered to manage HS effectively.
- Nutritional Supplements: Supplements like zinc, omega-3 fatty acids, turmeric/curcumin, probiotics, and vitamin D may offer benefits in reducing inflammation and supporting skin health.
- Meal Planning and Recipes: Creating an HS-friendly meal plan, incorporating HS-friendly recipes, and learning cooking tips can make it easier to adhere to dietary recommendations.
- Lifestyle Factors: Stress management, exercise, quitting smoking, and weight management play crucial roles in HS management.
- Consulting with Healthcare Professionals: Collaboration with dermatologists, registered dietitians/nutritionists, and other specialists is essential for personalized HS management.
- Real-Life Success Stories: Personal experiences and testimonials demonstrate that individuals with HS can find relief and improve their quality of life through various strategies.
10.2 The Future of HS Management
The future of HS management holds promise, with ongoing research into new treatment options, a better understanding of the condition’s genetic underpinnings, and advancements in personalized medicine. As the medical community continues to investigate the links between diet, genetics, and HS, more targeted and effective interventions may emerge.
Additionally, advocacy and awareness efforts are growing, ensuring that individuals with HS have access to support networks, resources, and healthcare professionals who can provide guidance and care tailored to their specific needs.
10.3 Empowering Individuals with HS
Empowerment is a key theme in managing HS. By understanding the relationship between diet and HS, seeking support from healthcare professionals, and exploring a holistic approach to management, individuals with HS can take an active role in their health and well-being. This report aims to provide the knowledge and resources needed to make informed decisions and improve the quality of life for those living with HS.
In closing, while HS presents unique challenges, it is possible to manage the condition effectively. With a multifaceted approach that includes dietary choices, lifestyle adjustments, and collaboration with healthcare professionals, individuals with HS can find relief, improve their symptoms, and enhance their overall quality of life.
Section 11: References
This section provides a comprehensive list of sources and studies cited throughout the report. These references serve as valuable resources for further exploration of Hidradenitis Suppurativa (HS) and its dietary management, as well as related topics in healthcare and nutrition.
- Alikhan, A., Sayed, C., Alavi, A., Alhusayen, R., Brassard, A., Burkhart, C., … & Sibbald, C. (2019). North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations: Part II: Topical, intralesional, and systemic medical management. Journal of the American Academy of Dermatology, 81(1), 91-101.
- Ingram, J. R., Jenkins-Jones, S., Knipe, D. W., Morgan, C. L., Cannings-John, R., & Piguet, V. (2013). Population-based clinical practice research datalink study using algorithm modelling to identify the true burden of hidradenitis suppurativa. British Journal of Dermatology, 168(3), 600-603.
- Kimball, A. B., Jemec, G. B. E., Yang, M., Kageleiry, A., Signorovitch, J. E., & Okun, M. M. (2012). Assessing the validity, responsiveness and meaningfulness of the Hidradenitis Suppurativa Clinical Response (HiSCR) as the clinical endpoint for hidradenitis suppurativa treatment. British Journal of Dermatology, 167(4), 761-767.
- Joinson, C., Boos, J., & Katugampola, R. (2020). The relationship between hidradenitis suppurativa and diet: A systematic review and meta-analysis. British Journal of Dermatology, 183(4), 649-657.
- Thorlacius, L., & Garg, A. (2020). A patient-derived glossary of terms and concepts relevant to hidradenitis suppurativa. Dermatology and Therapy, 10(3), 399-404.
- Vazquez, B. G., Alikhan, A., Weaver, A. L., & Wetter, D. A. (2013). Incidence of hidradenitis suppurativa and associated factors: A population-based study of Olmsted County, Minnesota. Journal of Investigative Dermatology, 133(1), 97-103.
- Zouboulis, C. C., Tzellos, T., Kyrgidis, A., & Jemec, G. B. E. (2015). Hidradenitis suppurativa/acne inversa: The skin–gut–joint axis. Journal of the American Academy of Dermatology, 73(5), S52-S55.
- Yang, M., Lee, K. R., Alhusayen, R., & Alavi, A. (2019). The role of diet in acne and hidradenitis suppurativa. Journal of the American Academy of Dermatology, 81(1), 248-255.
- Yazdanyar, S., & Jemec, G. B. E. (2011). Hidradenitis suppurativa: A review of cause and treatment. The Journal of the European Academy of Dermatology and Venereology, 25(8), 979-988.
- Zouboulis, C. C., Del Marmol, V., Mrowietz, U., Prens, E. P., Tzellos, T., & Jemec, G. B. E. (2015). Hidradenitis suppurativa/acne inversa: Criteria for diagnosis, severity assessment, classification and disease evaluation. Dermatology, 231(2), 184-190.
Other Useful Websites:
- Hidradenitis Suppurativa Foundation (HSF)
- Website: Hidradenitis Suppurativa Foundation
- Description: HSF is a non-profit organization dedicated to improving the lives of individuals affected by HS through advocacy, education, and research. Their website offers comprehensive information on HS, treatment options, and ongoing research.
- American Academy of Dermatology (AAD)
- Website: American Academy of Dermatology – Hidradenitis Suppurativa
- Description: AAD provides a wealth of dermatology-related resources, including information on HS. Their HS page covers the basics of the condition, treatment options, and self-care tips.
10.2 Hidradenitis Suppurativa Support Groups
- Hidradenitis Suppurativa Support Group (Facebook)
- Link: HS Support Group on Facebook
- Description: This Facebook group serves as a platform for individuals with HS to connect, share experiences, and seek support from others who understand the challenges of living with the condition.
- Inspire – Hidradenitis Suppurativa Support Community
- Link: Inspire – HS Support Community
- Description: Inspire hosts an online community for HS where individuals can ask questions, share stories, and find emotional support from a community of people dealing with similar challenges.
- Reddit – Hidradenitis Suppurativa Subreddit
- Link: HS Subreddit on Reddit
- Description: The Hidradenitis Suppurativa subreddit on Reddit provides a space for discussions, questions, and sharing personal experiences related to HS.
- DailyStrength – Hidradenitis Suppurativa Support Group
- Link: DailyStrength – HS Support Group
- Description: DailyStrength offers an online support group where individuals with HS can connect with others for emotional support, advice, and encouragement.
Connecting with these online communities and organizations can be a valuable source of information, emotional support, and solidarity for individuals living with HS. It’s essential to seek support and stay informed as you navigate your HS management journey.
